Shin Splints in Runners: Causes, Treatment & 5‑Day Recovery Plan
If you’ve felt that sharp, nagging ache down the front of your lower leg mid‑run—the kind that makes you question the next step—you’re not alone. Almost every runner meets shin splints at some point. The good news? With a little rest, the right strength moves, and a smart plan, you can calm the fire and come back stronger.
“Running is life, not numbers. This plan helps you stay kind to your body while you heal.”
The Mental Health Side of Shin Splints
Runners are wired to keep pushing. When the plan says “5 miles,” most of us feel uneasy stopping at four, even when our shins are screaming. We worry about losing fitness, falling behind, or letting our team—or ourselves—down.
But here’s the truth: pushing through pain rarely makes you stronger. It usually makes the injury louder. Shin splints are your body’s way of asking for attention, not punishment.
The mental battle of rest is real. Many runners tell me they feel anxious or irritable when they can’t run—it’s part of why running feels so vital to mental health. When pain forces us to pause, it can feel like losing a coping mechanism. That’s why it’s important to reframe recovery: you’re not stepping back; you’re choosing long-term health over short-term relief.
Try this during downtime:
Walk or cross-train outdoors to keep your mental rhythm.
Journal about how your body feels each day.
Remember that consistency over years—not one perfect training block—is what builds real strength.
Healing isn’t quitting. It’s the deepest kind of discipline.
What Exactly Are Shin Splints?
Plain‑English definition: Pain along the tibia (shin bone) where the lower‑leg muscles and tendons—especially the tibialis anterior and soleus—get irritated from overuse.
Why they show up:
Big, sudden jumps in mileage or speed
Worn‑out or poorly matched shoes
Overstriding or heavy heel striking
Not enough calf/ankle strength and mobility work
Red‑flag check: If pain lives on one tiny pinpoint, hurts at rest or at night, or spikes with a hop test, press pause and see a clinician to rule out a stress fracture.
Common Symptoms
Dull ache or tenderness along the inner/front shin
Mild swelling or warmth
Worse with running, eases with rest
Soreness with foot flexion or when pressing the area
Treatment That Actually Works
Reduce impact for 3–5 days. Swap in walking, cycling, or pool running.
Ice 15–20 minutes, 2–3×/day. Use a barrier between skin and ice.
Gentle soft tissue. Foam roll calves; light lacrosse ball massage along the shins (avoid pressing directly on bone).
Strength + mobility. Daily calf raises, toe lifts, ankle circles (see exercises below).
Shoe/Surface check. Retire tired shoes; favor softer paths for a few weeks.
Coach tip: Keep pain ≤ 3/10. If it rises, back off a day and breathe.
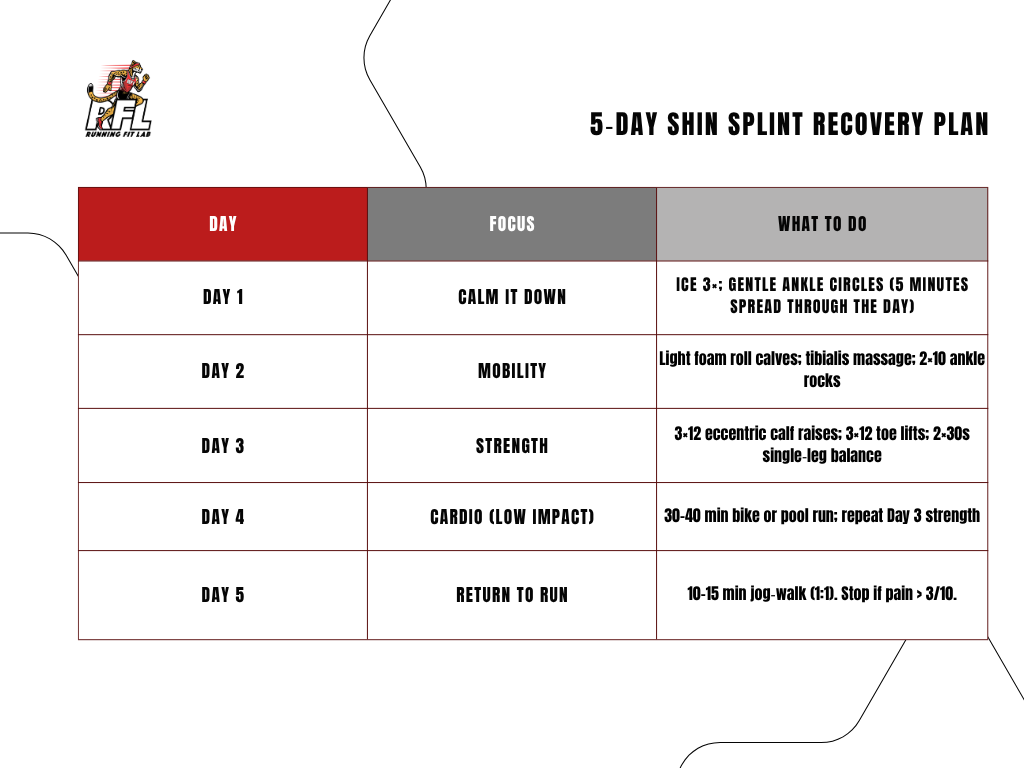
5‑Day Shin Splint Recovery Plan
Use this reset, then test a short jog‑walk. If pain climbs above 3/10, repeat the last pain‑free day.
3 Exercises to Fix Shin Splints (Daily)
Eccentric Calf Raises — 3×12 each side; slow down for a 3‑count.
Toe Curls with Towel — 2×60s; focus on foot arch control.
Single‑Leg Balance on Soft Surface — 2×30–45s each; progress by closing eyes or adding light knee drive.
Before/After: Sarah’s Comeback
Before: Sarah from Pleasanton doubled her weekly mileage and finished every run with sharp shin pain. We scaled back, added daily calf work, and moved her easy miles onto softer surfaces.
After: Eight weeks later she finished the Livermore Valley Half comfortably—pain‑free and grinning at the finish line.
Helpful Classes & Coaching
Strength Training for Runners — Join a class
Personal Coaching — One‑on‑One support
Custom “Injury Comeback” Plan
FAQ
-
Usually training spikes, under‑prepared lower‑leg muscles, and form issues like overstriding. Shoes matter, too.
-
Mild cases often settle in 1–2 weeks with reduced impact and daily strength/mobility. Recurring or severe cases can take 3–4+ weeks.
-
If pain is low (1–3/10) and trending better, short jog‑walks are okay. Sharp or worsening pain? Stop and switch to low‑impact cardio.
-
Pinpoint pain, night pain, swelling that doesn’t settle, or no improvement with rest—get evaluated to rule out a stress fracture.